Stop the spread: Infection management at home of care receiver
- CareBuddy
- 4 Mins Read
- 11 Oct 2022
- Infection Control

An infection is an intrusion of a pathogenic (disease-causing) microorganism into the body, where it can damage physical tissues and physiological functions of the body, leading to diseases and an overall decrease in wellness. Common infectious agents include bacteria, fungi and viruses. A care receiver who’s infected with one of these pathogens is called a host.
Major infection routes and common infections that are spread through each route include
Contact infection
A transmission route with high frequency of transmission. Mostly through fingers, food and apparatus.
Examples: Norovirus, Methicillin-resistant Staphylococcus aureus (MSRA), Pseudomonas aeruginosa
Droplet infection
Through inhalation of droplets of a cough or sneeze. Happens within 1 minute of droplet expulsion as the droplets fall on the floor after that.
Examples: Influenza, epidemic parotitis, rubella, Legionella bacteria
Airborne infection
Developed through inhalation of a pathogen while it’s suspended in the air for a long time.
Examples: Tuberculosis, measles, chickenpox
Percutaneous infection
When a pathogen enters the body through a wound, bite or sting by a mosquito or any other insect or animal.
Examples: Malaria, dengue, Japanese encephalitis
Blood-mediated infection
When blood, blood fluid or other secretions are contaminated with a pathogen that enters through a needle prick or similar.
Examples: Hepatitis B, Hepatitis C, HIV
The chain of infection (also known as chain of transmission) of an infectious disease
- Infectious Agent
This is the pathogen that causes infection.
Examples: Bacteria, Fungi, Viruses, Parasites - Reservoirs
These are the places where the pathogen is stored.
Examples: People, Water, Food - Portals of Exit
These are the ways through which the pathogen can escape from its reservoir.
Examples: Blood, Secretions, Excretions, Skin - Modes of Transmission
These are the ways in which the pathogen can be transmitted.
Examples: Contact, Droplet, Airborne - Portals of Entry
These are the ways through which the pathogen can enter a host.
Examples: Respiratory, Gastrointestinal, Broken Skin - Susceptible Host
A care receiver who’s particularly vulnerable to getting infected with a pathogen.
Examples: People with diabetes, burns, surgery, advanced age or any other factor that can weaken immune system.
Infection prevention measures broadly fall into 3 categories:
- Removing the infection source
- Breaking the chain of infection
- Enhancing the host’s resistance
Removing the infection source
Remove all possible sources of infection such as
- Vomit
- Excreta (urine, stool)
- Blood and any other body fluid (e.g. sputum, pus)
- Used appliances (e.g. injection needle, gauze)
- Food handled by fingers contacting the above
Wear gloves when handling the above. After removing gloves, remember to wash hands and disinfect fingers.
Breaking the chain of infection
Sometimes it’s not feasible to remove the source of infection. If so, there are ways to break the chain of infection such as
- Enforcing regular handwashing with warm water and soap
- Cleaning the environment as frequently as possible
- Wearing appropriate gloves
- Wearing masks, aprons or gowns to further reduce chances of spread
- Observe cough and respiratory etiquette, e.g. don’t cough, sneeze or blow near another person
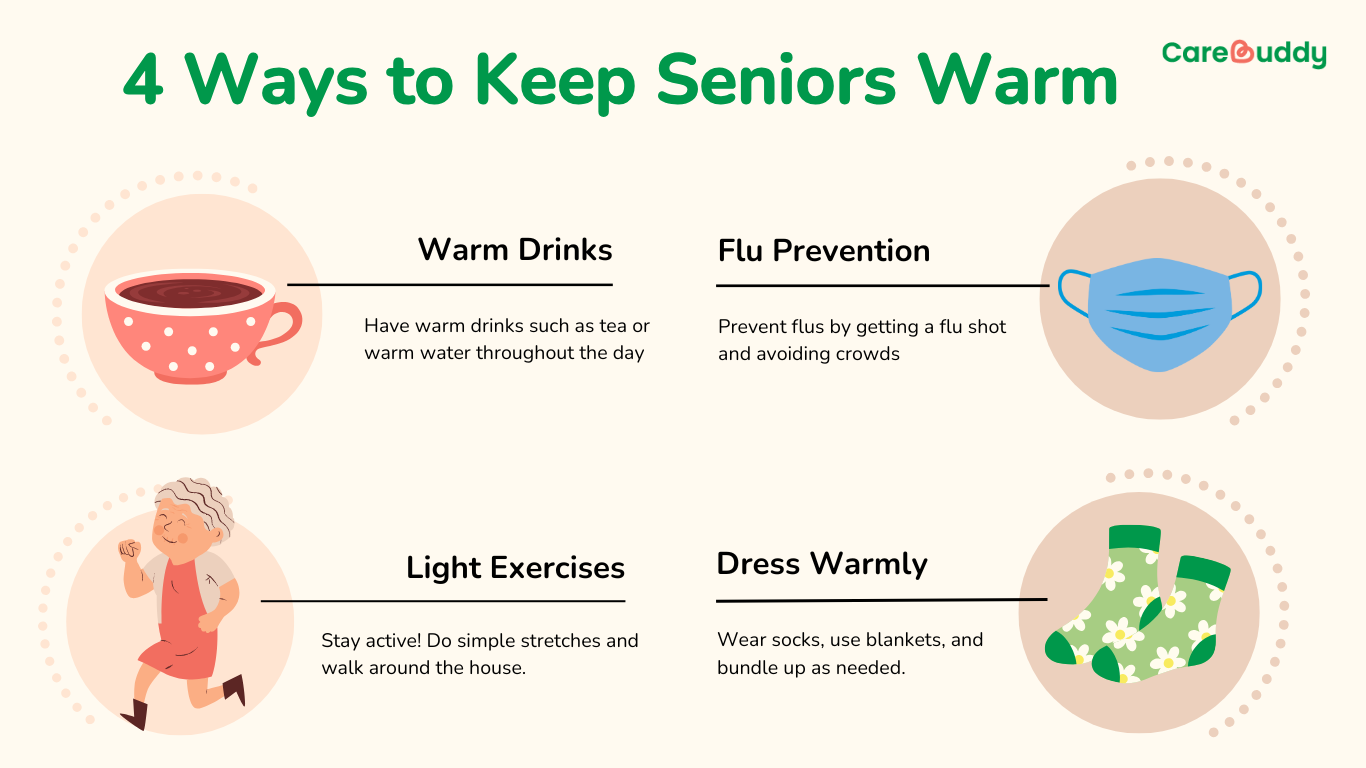
Enhancing the care receiver’s resistance
The care receiver’s ability to withstand infection can be strengthened by
- Getting flu shots and other recommended vaccines regularly
- Maintaining a healthy diet
- Exercising regularly
- Staying hydrated with 7 to 8 glasses of water a day
- Sleeping 7 to 8 hours a day
- Reducing stress
Article reviewed by David Tay, Senior Principal Educator (Nursing and Prehospital Care), HMI Institute.